Abstract
Purpose
To report histopathologic changes of the ocular surface pannus in patients with severe limbal stem cell deficiency (LSCD).
Methods
Corneal and conjunctival pannus tissues from 29 patients undergoing ocular reconstruction with cultured limbal cell transplantation were included. The medical records of these patients were reviewed for demographics, aetiologic diagnosis, type of injury, interval between the initial insult and excision of pannus, and medical history involving human amniotic membrane (HAM) or limbal transplantation. The paraffin-embedded tissues were reviewed for epithelial changes, type–degree of fibrosis, degenerative changes, vascular changes, conjunctivalization of corneal surface, and evidence of residual HAM. We attempted a clinicopathologic correlation to understand the pathogenesis of pannus formation in LSCD.
Results
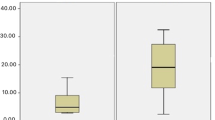
The 29 tissues were from 29 eyes of patients with primary aetiology of chemical burn in 89.6% (undetermined in 10.4%) of cases. The pannus showed epithelial hyperplasia in 62%, active fibrosis in 66%, severe inflammation in 21%, giant cell reaction in 28%, and stromal calcification in 14% cases. Goblet cells were seen over the cornea in 64% cases; their absence was associated with squamous metaplasia of the conjunctiva and with long duration of insult. Evidence of residual HAM was noted in 42% cases.
Conclusions
The commonest cause of severe LSCD is alkali-induced injury. Goblet cells over the cornea were seen in 60% of cases. HAM used for ocular surface reconstruction could persist for long periods within the corneal pannus, thus raising the need for further studies with long-term follow-up.
Similar content being viewed by others
Introduction
Severe ocular surface disease is a clinical term applied to conditions resulting from injury or disease of either limbal stem cells (which form the source of regenerating the corneal epithelium) and/or the conjunctiva (which harbours the mucin-secreting goblets cells) that are essential for an ocular surface integrity.1, 2 The common conditions leading to either loss or hypofunction of limbal stem cells include chemical or thermal burns, Stevens–Johnson disease, ocular cicatrizing pemphigoid, multiple surgeries, and conditions that could lead to insufficient stromal microenvironment to support stem cell function including aniridia, congenital erthrokeratodermia, neurotrophic keratitis, or chronic limbitis.3, 4, 5 The disease manifests as epithelial defects, chronic inflammation, keratitis, vascularization, and fibrosis, ultimately resulting in corneal blindness. The newer modalities of treatment developed apart from conventional techniques of keratectomy, lamellar or penetrating keratoplasty, include epithelial transplantation procedures like limbal, kerato-limbal, or cultured corneal epithelial transplantation.6, 7, 8, 9, 10, 11, 12, 13, 14, 15, 16, 17 At our centre, patients clinically diagnosed with severe ocular surface disease due to limbal stem cell deficiency, with or without associated conjunctival damage, are treated with cultured corneal epithelium after surgical debridement of the diseased ocular surface pannus. We observed some unusual findings in the excised diseased ocular surface pannus among recipients of cultured epithelium, which prompted us to undertake a detailed histopathologic study of these tissues. To the best of our knowledge, no such study has been reported previously (Medline search).
Materials and methods
We retrospectively reviewed the excised ocular surface tissue submitted to the ophthalmic pathology service at a tertiary referral eye care centre from patients undergoing cultured epithelial transplantation procedures. The medical records of the patients were reviewed with special reference to clinical diagnosis, primary insult, duration of insult, any surgical intervention before the cultured limbal stem cell transplantation procedures, use of amniotic membrane for surface reconstruction, and any other associated features.
Before transplanting the amniotic membrane with cultured corneal epithelial cells, the recipient bed was prepared by removing the unhealthy tissue over the ocular surface. The surgeries were performed either under local or general anaesthesia (in children below 14 years). In brief, 360° annular conjunctival peritomy was performed starting 4–5 mm from limbus, following which dissection was continued towards the limbus using Tenotomy scissors. The conjunctival tissue was excised at the limbus. The corneal pannus was dissected either in toto, or piecemeal, dissecting sharply along planes of cleavage using a #15 Beaver blade mounted on a Bard Parker handle. The sections from the formalin-fixed, paraffin-embedded tissues were stained with haematoxylin and eosin, and periodic acid Schiff's stain. Special staining (eg, Alcian blue) was carried out in a few cases to detect the remnants of AMG. The sections were then evaluated for histologic changes in the epithelium and stroma, namely presence of goblet cells, hyperplasia, keratinization, inflammation, fibrosis, giant cell reaction, calcification, and residual amniotic membrane if applied earlier. In most cases, the excised pannus over the corneal and conjunctival region was submitted separately and therefore could be evaluated separately. In cases where the corneal and conjunctival tissues were submitted together, the data were included for evaluation of changes involving the entire ocular surface changes only. The results were correlated using Pearson's χ2 and Fisher's exact test.
Immunohistochemistry of excised pannus
Immunohistochemical analysis was performed on paraffin-embedded sections of pannus using monoclonal antibody AE5 specific for cytokeratin K3 to confirm the phenotype of epithelial cells. The paraffin sections were de-waxed by heat treatment, followed by subsequent washing in xylene and absolute alcohol. The endogenous peroxidase activity was blocked by washing the sections with hydrogen peroxide–methanol solution (3%). The nonspecific antigenic sites were then blocked by washing the sections with bovine serum albumin. The specimen was then incubated with primary antibody AE5 (ICN Biochemicals) followed by subsequent incubations with secondary antibody conjugated with horseradish peroxidase and avidin–biotin complex, respectively. Finally, the antigen–antibody reactions were determined by colour reaction with 3 3′-diamino benzidine (DAB). At each step, the sections were washed with 1 × PBS.
Results
We studied ocular surface pannus from 29 eyes of 29 patients who underwent ocular surface reconstruction with cultured corneal epithelium. The mean age of patients was 18 years (range 2–36 years), with a male to female ratio of 5 : 1. Children under 15 years constituted 38% of the cases. Clinical diagnosis of severe limbal stem cell deficiency was made in all cases. This was associated with symblepharon in 9 (31%) cases. The primary aetiology in these cases was chemical burns in 26/29 cases (17 alkali-induced, 6 acid-induced, 3 unknown chemical) and vernal keratoconjunctivitis in 1 case. The aetiology was unknown in two cases. Of the 20 cases of alkali injury, 13 were due to lime, while 2 were due to caustic soda; 1 case each was due to sodium hydroxide and caustic lye. The mode of injury was reported to be accidental in all cases, acquired at home in 5/26 cases and industrial in 7/26 cases. No information was available in 14/26 cases.
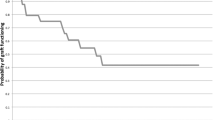
The mean time lapsed from injury to the transplantation procedure was 25 months (ranging from 2 to 77 months). Most of the patients consulted an ophthalmologist for treatment within a few minutes to a few hours after the injury. The previous surgeries performed in these patients included amniotic membrane grafting in 12 (41%), penetrating keratoplasty in 4 cases, symblepharon release in 4 cases, limbal transplantation in 3 cases, pannus resection in 2 cases, and lamellar keratectomy in 2 cases.
In 23 cases, the excised pannus over the corneal and conjunctival region was submitted separately, while in 6 cases, the tissues were submitted together. In one case, the corneal epithelium was absent and the surface was covered by necrotic stroma.
The histologic spectrum of changes in the 29 excised tissues is shown in Table 1. The extent of epithelial hyperplasia varied across cases with complete necrosis in one case. Evidence of squamous metaplasia of ocular surface in the form of presence of keratinization or reduced conjunctival goblet cells was noted in 10 (34%) cases (Figure 1). Varying amounts of fibrocollagenous stroma were noted in the subepithelial region (Figure 2). Many cases showed active fibrosis (19; 66%) with increased number of fibroblasts containing a plump, vesicular nucleus. Severe inflammation mostly consisting of lymphoplasmacytic infiltrates (Figure 3) admixed with eosinophils and mast cells was seen in 14 (48%) cases. Evidence of multinucleated giant cells (Figure 4) within the stroma was noted in eight (28%) cases. Stromal calcification (Figure 5) consisting of bluish concentric deposits was seen in four (14%) cases. In five cases, there was a thick wavy band-like membrane in the subepithelial region, highly suggestive of residual amniotic membrane (Figure 6a and b). In three cases, there was a neutrophilic infiltrate around the membrane, suggesting an attempt at phagocytosis of the membrane. Alcian blue staining in these cases revealed a pale blue staining of the membrane.
(a) Histologic section of the corneal region of the pannus showing a multilayered epithelium. Note the underlying thick, wavy, pale eosinophilic, acellular membrane (arrows) in the subepithelial stroma with a few neutrophils in close approximation, highly suggestive of the residual amniotic membrane (haematoxylin and eosin, × 250). (b) Sections from another membrane showing similar membrane highly reminiscent of the residual amniotic membrane (periodic acid Schiff's stain, × 250).
The comparison between the histologic changes in corneal and conjunctival region (Table 1) revealed that there was more dense fibrosis in the cornea, with evidence of conjunctivalization in 64% (14/22) cases (Figure 7) and evidence of residual AMG in four cases. Evidence of conjunctivalization (ingrowth of thickened fibrovascular pannus, abnormal fluorescein staining, goblet cells on impression cytology of cornea region) was noted in patients who received previous surgical treatment (8/14), as well as in those who did not receive any treatment (6/14). There was however no statistically significant difference (Table 1) in the changes seen over cornea or conjunctiva, except for the presence or absence of residual amniotic membrane in patients earlier treated with amniotic grafting.
Discussion
The common causes of secondary limbal stem cell deficiency include chemical and thermal burns, Stevens–Johnson syndrome, ocular cicatrizing pemphigoid, multiple surgeries or cryotherapies, contact lens wear, and microbial infections.3, 4, 5, 6 The diagnosis of LSCD is usually based on the cumulative evidence gathered by history (photophobia, tearing, blepharospasm, recurrent attacks of pain, history of chronic redness, and inflammation), clinical findings (loss of palisades of Vogt, dull and irregular corneal epithelium with loss of transparency), and evidence of conjunctivalization.3, 4, 5, 9 In our experience, some cases of clinically diagnosed LSCD failed to reveal goblet cells on impression cytology; instead they showed evidence of squamous metaplasia of the entire ocular surface. So, an effort was made to study the histopathology of the excised pannus in order to get an insight into pathogenesis of chemical burns.
Similar to other reported series of chemical burns, the affected individuals are young with a mean age of 18 years (2–36 years), with 38% cases affecting children less than 15 years of age. The commonest cause of limbal stem cell deficiency requiring active surgical intervention was chemical injury (26/29; 90%). A majority of these were due to alkali burns (20/26; 77%) affecting predominantly the males, as reported by others.18, 19 Lime is not only used as a whitewashing agent in detergents, but is also applied on the betel leaf to prepare ‘paan’ (eaten by many Indians). The easy availability of lime in households, made more appealing by being packed in convenient sachets, explains the high frequency of household accidents involving this chemical in children.
The severity of ocular injury after chemical injury depends on the surface area of contact and the degree of penetration. Alkali penetrates tissues to a greater extent than does acid.20, 21 Depending on their penetration, the chemical burns can result in necrosis of the ocular surface, leucocytic infiltration, or prolonged inflammation, which leads to damage of the ocular surface epithelium as well as the stromal tissues.22, 23, 24 Loss of vascularity to the limbus results in necrosis of cornea, and the decrease in collagenase inhibitors leads to stromal destruction, ulceration, and perforation. The long-term damage to the ocular surface includes distortion and dysfunction of proximal or distal bulbar conjunctiva, tarsal conjunctiva, and the anterior orbital tissues, thereby resulting in abnormalities in surface mucous secretion and surface wetting, cicatrizing of conjunctiva, symblepharon, and entropion.20, 21 Many patients in this series had washed their eyes at home, before attending the ophthalmologist's clinic for first aid; despite this, all these patients developed severe surface damage.
McCulley20 divided the clinical course of chemical injury into four distinct pathophysiologic and clinical phases: the immediate, acute (0–7 days), early repair (7–21 days), and late repair (more than 21 days). If we apply the limbal stem cell injury model to the chemical injuries: grade I injury involves little or no loss of stem cells; grade II involves subtotal stem cell loss; grade III has complete stem cell loss with retention of some proximal conjunctival epithelium and vascularity; and grade IV injury involves complete loss of stem cells and loss of proximal conjunctival epithelium, with or without associated damage to anterior segment. Although we do not have the clinical details of the degree of chemical injury and the changes observed in the acute phase, based on the history and the literature-based evidence of clinical course and pathophysiology of chemical burns,22 we assume that these cases with a fibrovascular pannus formation represent type III of the late-phase repair process. The fibrovascular pannus, which gives tectonic support to the eye and prevents stromal melt and perforation, could also lead to visual loss. Tissues from patients with this condition provide proof of the chronic changes on the ocular surface after chemical burns. Additional clinical evidence of conjunctival cicatrization and symblepharon was found in 9 (31%) cases. The limitation of the existing classification of chemical burns has paved the way for a new classification system that takes into account not only the extent of limbal involvement in clock hours, but also the percentage of conjunctival involvement.25 It would be logical to presume that the clinical and morphologic features of the ocular surface in isolated limbal damage would differ from cases with damage to limbus and conjunctiva. None of these cases had an abnormality of the anterior segment or intraocular structures, and were therefore considered for surgical reconstruction of the ocular surface with cultured corneal epithelium.
Overall, histologic changes observed in the ocular surface pannus included epithelial hyperplasia (62%), squamous metaplasia (34%), active stromal fibrosis (66%), severe inflammation (48%), and evidence of calcification with giant cell reaction (28%). Since this is a retrospective study and includes cases presenting at various stages of clinical course, either before or after any surgical intervention, it was not possible to correlate the histologic changes to any specific aetiologic cause. In all these cases except one, there was evidence of complete re-epithelization of the corneal surface by stratified squamous cells, which showed varying degrees of squamous metaplasia and keratinization. Evidence of goblet cells on the corneal region of the pannus was noted in 14 (64%) cases, both in the treated and untreated group. In the cases that did not show evidence of goblet cells over the cornea, there was a reduction in the number of goblet cells over the conjunctival surface as well, suggesting changes in the entire ocular surface. In a study by Puangsricharern and Tseng,4 impression cytology from 137 cases of clinically suspected LSCD (based on evidence of chronic inflammation, scarring, and vascularization) showed evidence of conjunctivalization of cornea in 94 (70%) cases; 40 cases showed no evidence. They suggested that the absence of goblet cells in this subset of patients (including two cases of acid burn) could represent a subclinical stage of LSCD, a partial form of LSCD, or could be due to the insensitivity of this test to pick up early cases. They proposed that the evidence of goblet cells over the cornea is the hallmark of conjunctivalization and therefore confirms the diagnosis of limbal stem cell deficiency. However, our interpretation is that the presence of goblet cells does confirm the diagnosis of LSCD, but their absence does not exclude the diagnosis, especially in cases of severe LSCD secondary to chemical burns where the entire ocular surface is damaged. We do find support for this hypothesis in some studies that have shown a decrease in the goblet cell density within the conjunctiva in chemical burns.26 Moreover, most of the data on wound healing in chemical burns are obtained from animal experiments, wherein the limbus is selectively damaged with chemicals to produce limbal stem cell deficiency. However, in human eyes, ocular surface insult from chemical burns may go beyond damage to the limbal tissues.
Evidence of calcification was noted in four cases at a mean interval of 4 months after injury. These deposits, seen mostly in deep stroma, could either be residual calcium deposits after lime injury or the calcification of soaps as observed in certain animal experiments. It is however beyond the scope of this study to confirm the nature of the residual amphophilic deposits in the ocular tissues after chemical burns.
Evidence of residual amniotic membrane in the excised pannus noted in 42% (5 of 12) patients who received AMG is an interesting finding. Although we did not use any specific marker to detect the AMG, the morphological appearance of the pale PAS-positive, Alcian blue-positive elongated structure surrounded by neutrophilic infiltrates was highly suggestive of residual AMG. We also noted that there was greater evidence of residual AMG on the corneal surface than on the conjunctival surface; this suggests that the conjunctival dissolution of the membrane is faster than in the corneal region. This is not only of academic interest, but could have long-term implications on the use of cultured epithelium using amniotic membrane as a carrier. Long-term follow-up of these patients, histologic study of the excised tissues, and keratoplasty specimens could help us understand the rate of dissolution of this membrane in the cornea.
Chemical burns invariably cause damage to the surface epithelium as well as to the stromal matrix. The persistence of active fibroblasts in some of the tissues is a proof of ongoing stromal changes, long after the primary damage from chemical burns. The initial influx of polymorphonuclear cells and direct damage of the stromal matrix and fibroblasts could possibly trigger off a vicious cycle of inflammation, wound repair, and fibrosis, thus masking specific changes, if any, of the primary insult.
In summary, alkali burns are the commonest cause of severe LSCD, producing long-standing and persistent changes like epithelial hyperplasia, fibrosis, and inflammation over the ocular surface. Amniotic membrane if used in ocular surface reconstruction could persist for long periods within the corneal pannus. Goblet cells on cornea confirm the diagnosis of LSCD, but their absence does not rule out LSCD, and correlates with prolonged interval and squamous metaplasia of the entire surface in such cases.
References
Holland EJ . Epithelial transplantation for the management of severe ocular surface disease. Trans Am Ophthalmol 1996; 94: 677–743.
Croasdale CR, Schwartz GS, Malling JV, Holland EJ . Keratolimbal allografts: recommendations for tissue procurement and preparation by eye banks, and standard surgical technique. Cornea 1999; 18: 52–58.
Tseng SC . Concept and application of limbal stem cells. Eye 1989; 3: 141–157.
Puangsricharern V, Tseng SCG . Cytologic evidence of corneal diseases with limbal stem cell deficiency. Ophthalmology 1995; 102: 1476–1485.
Dua HS, Azuara-Blanco A . Limbal stem cells in corneal epithelium. Surv Ophthalmol 2000; 44: 415–425.
Tsai RJ, Li L, Chen J . Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med 2000; 343: 86–93.
Dua HS, Azuara-Blanco A . Autologous limbal transplantation in patients with unilateral corneal stem cell deficiency. Br J Ophthalmol 2000; 84: 273–278.
Tsubota K, Toda I, Saito H, Shinozaki N, Shimazaki J . Reconstruction of the corneal epithelium by limbal allograft transplantation for severe ocular surface disorders. Ophthalmology 1995; 102: 1486–1496.
Tsai RJ, Tseng SCG . Human allograft limbal transplantation for corneal surface reconstruction. Cornea 1994; 13(5): 389–400.
Tan DT, Ficker LA, Buckley RJ . Limbal transplantation. Ophthalmology 1996; 103: 29–36.
Rao SK, Rajagopal R, Sitalakshmi G, Padmanabhan P . Limbal allografting from related live donors for corneal surface reconstruction. Ophthalmology 1999; 106: 822–828.
Pellagrini G, Traverso EC, Franzi TA . Long-term restoration of damaged corneal surfaces with autologus cultivated corneal epithelium. Lancet 1997; 349: 990–993.
Scwab IR . Cultured corneal epithelia for ocular surface disease. Trans Am Ophthalmol Soc 1999; 97: 891–986.
He YG, Alizadeh H, Kinoshita K, McCulley JP . Experimental transplantation of cultured human limbal and amniotic epithelial cells onto the corneal surface. Cornea 1999; 18: 570–579.
Tsai RJ, Li LM, Chen JK . Reconstruction of damaged corneas by transplantation of autologous limbal epithelial cells. N Engl J Med 2000; 343: 86–93.
Ivan R, Schwab MD, Merle R . Successful transplantation of bioengineered tissue replacements in-patients with ocular disease. Cornea 2000; 19(4): 421–426.
Koizumi N, Inatomi T, Suzuki T, Sotozono C, Kinoshita S . Cultivated corneal epithelial stem cell transplantation in ocular surface disorders. Ophthalmology 2001; 108: 1569–1574.
Wagoner MD . Chemical injuries of the eye: current concepts in pathophysiology and therapy. Surv Ophthalmol 1997; 41: 275–313.
Morgan SJ . Chemical burns of the eye: causes and clinical management. Br J Ophthalmol 1987; 71: 854–857.
McCulley JP . Chemical injuries. In: Smolin G, Thoft RA (eds). The Cornea: Scientific Foundations and Clinical Practice, 2nd ed. ittle, Brown and Co.: Boston, 1987, pp 527–542.
Grant WM, Kern HI . Action of alkalies on the corneal stroma. Arch Ophthalmol 1955; 54: 931–934.
Kenyon KR, Berman M, Rose J, Gage J . Prevention of stroma ulceration in the alkali burned rabbit cornea by glued on contact lens. Evidence of role of polymorphonuclear leucocytes in collagen degradation. Invest Ophthalmol Vis Sci 1979; 18: 570–587.
Pfister RR . Chemical injuries of the eye. Ophthalmology 1983; 90: 1246–1253.
Paterson CA, Wells JG, Koklitis PA, Higgs GA, Docherty AJ . Recombinant tissue inhibitor of metalloproteases type- I suppresses alkali-burn induced corneal ulceration in rabbits. Invest Ophthalmol Vis Sci 1994; 35: 677–684.
Roper-Hall MJ . Thermal and chemical burns. Trans Ophthalmol Soc UK 1965; 85: 631–653.
Dua HS, King AJ, Joseph A . A new classification of ocular surface burns. Br J Ophthalmol 2001; 85: 1379–1383.
Acknowledgements
This work was funded by the Hyderabad Eye Research Foundation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fatima, A., Iftekhar, G., Sangwan, V. et al. Ocular surface changes in limbal stem cell deficiency caused by chemical injury: a histologic study of excised pannus from recipients of cultured corneal epithelium. Eye 22, 1161–1167 (2008). https://doi.org/10.1038/sj.eye.6702895
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702895
Keywords
This article is cited by
-
The biophysical property of the limbal niche maintains stemness through YAP
Cell Death & Differentiation (2023)
-
Understanding Ocular Surface Inflammation in Tears Before and After Autologous Cultivated Limbal Epithelial Stem Cell Transplantation
Ophthalmology and Therapy (2023)
-
Mucous membrane grafting (fibrin glue vs. suture) for lid margin pathologies in Stevens–Johnson syndrome: randomized comparative study
Eye (2021)
-
Spectral-domain optical coherence tomography for evaluating palisades of Vogt in ocular surface disorders with limbal involvement
Scientific Reports (2021)
-
Assessment of corneal substrate biomechanics and its effect on epithelial stem cell maintenance and differentiation
Nature Communications (2019)