Abstract
Purpose
To investigate the clinical features and obtain guideline of treatment in intermittent exotropia associated with hypertropia including simulated superior oblique palsy.
Methods
We retrospectively reviewed the charts of 93 patients of intermittent exotropia aligned with horizontal muscle surgery only, who showed hypertropia more than 2 PD in primary gaze before surgery and disappeared after surgery. They showed forveal extorsion and dysfunction of oblique muscles of 2+ or less and positive Bielschowsky head tilt test. The postoperative changes of deviation angle were analysed at postoperative 1 day, 6 months, and 1 year.
Results
Average amount of distant horizontal deviation in primary gaze was 32.3±9.58 (25–53) PD, hypertropia was 3.50±2.52 (2–14) PD. Average vertical deviation of ipsilateral (hypertropic eye) side was 8.8±4.63 PD and contralateral (hypotrophic eye) side was 4.0±4.77 PD in Bielschowsky head tilt test. Hypertropic eye was accorded with exotropic eye in 53.4%. After horizontal surgery, the amount of hypertropia was 1.2 PD at postoperative 1 day. On Bielschowsky head tilt test, hypertropia was almost eliminated showing 0.6 PD on the ipsilateral side and 0.2 PD on the contralateral eye at 1 month. This state was maintained up to postoperative 1 year.
Conclusion
Small amount of hypertropia up to 14 PD in intermittent exotropia could be disappeared with horizontal muscle surgery only. However, careful examinations for head tilt history, fovea extorsion, oblique dysfunction, and Maddox rod test should be preceded to rule out true superior oblique palsy.
Similar content being viewed by others
Introduction
Intermittent exotropia is frequently associated with concomitant hypertropia. Overaction of oblique muscles and positive Bielschowsky head tilt test also manifest, which resembles superior oblique muscle palsy (SOP). The amount of hypertropia is variable. On many occasions, it ameliorates after obtaining horizontally aligned eyes by horizontal muscle surgery only without cyclovertical muscle surgery. However, surgeons frequently do combination of horizontal surgery and cyclovertical surgery and unnecessary cyclovertical surgery may induce another strabismus. We wonder how much amount of hypertropia disappear by only horizontal muscle surgery. Kushner1 reported seven patients of hypertropia with intermittent exotropia, who had mild oblique dysfunction. They did not show head tilt, cyclotropia, and SO underaction and he named it as simulated SOP.
In this study, the clinical features of hypertropia and postoperative outcomes after only horizontal muscles surgery were evaluated in patients with intermittent exotropia with hypertropia or simulated SOP, to give information on its treatment and prognosis.
Subjects and methods
The records of 93 patients were retrospectively reviewed. They had intermittent exotropia with hypertropia more than 2 PD in primary position, and obtained orthophoria after horizontal muscle surgery only without recurrence of hypertropia. Exclusion criteria were prominent foveal extorsion, +3 or +4 oblique dysfunction, contracture of superior rectus (SR) muscle on forced duction test, presence of head tilt or history, facial asymmetry, cyclodiplopia, history of cyclovertical muscle surgery, and reoperation.
The simulated SOP was defined when patient showed hypertropia more than 10PD in primary gaze, 2+ or less of SO underaction, overaction of inferior oblique (IOOA), and foveal extorsion, positive Bielschowsky head tilt testing without any history of head tilt, and disappearance of these symptoms after horizontal muscle surgery only.
General ophthalmic examination including estimation of visual acuity, cycloplegic refraction, and fundus examination was performed in all patients. The horizontal and vertical deviation in primary gaze, right and left gaze, up and down gaze, in the position with head tilt to the right and the left, was measured by prism and alternate cover test. Ocular version was assessed by observation as the patient followed visual target into cardinal position of gaze. Degree of foveal extorsion was estimated by fundus photographs. Dysfunction of the oblique muscles and foveal extorsion was graded on 1–4 scale. This quantitation was considered consistent because grading was performed by one examiner (YAC).
Sensory evidence of binocular vision was examined at near (Titmus-fly and Randot stereotest) and at distant (Mentor B-Vat II-SG videoacuity tester, USA) wearing polaroid glasses. Suppression was detected with Vectograph chart (projector type, Renau, France).
On the operating table, forced duction test was performed to detect the contracture of muscles. All patients underwent appropriate horizontal muscle surgery only (lateral recti recessions, recession, and resection in one eye, or three muscles surgery) by one surgeon (YAC). The pre- and postoperative changes of angle of deviation were analysed at postoperative 1 day, 1 month, 6 months, and 1 year (11.1±6.2 months in average).
Results
There were 46 male (49.4%) and 47 female patients (49.6%). Their age ranged from 5 to 19 years (11.4±7.2 years) of age. Fifty-six per cent of patients showed exotropia in the left eye and 41% of patients in the right eye. Alternate deviation was seen in 3% of the patients (Table 1). Mean amount of exotropia was 32.3±8.65 (25–53) PD, and average hypertropia was 3.5±1.60 (2–14) PD. Hypertropic eye was on the same side of exotropic eye in 53%, and on the side of fixating eye in 47% (Table 2).
Eighty-two per cent of patients showed positive Bielschowsky head tilt test. Average hypertropia on the hypertropic side was 8.8±4.63 (3–18) PD and on the nonhyperdeviating side 4.0±4.77 (0–16) PD. Positive Bielschowsky head tilt test was shown unilaterally in 50% of the patients, and bilaterally in 32% (Table 3). IOOA was +2 or less (average +1.18). SO dysfunction was almost none (average +0.23). There were no oblique dysfunctions of +3 or more. Simulated SOP was shown in 27 patients.
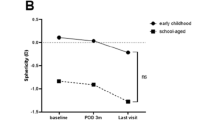
After horizontal muscle surgery only, the amount of horizontal deviation reduced to average 3.2±5.45 PD at postoperative 1 month. The amount of hypertropia was 1.2±1.81 (0–8) PD at postoperative 1 day and not more than 1 PD at 1 month, which did not appear again (Figure 1). The obtained orthophoria maintained up to follow-up of 1 year (Table 4).
Discussion
Small angle hypertropia and oblique dysfunction are frequently associated with exotropia patients. Hypertropia was noted in 40–63% of exotropes2, 3 and oblique dysfunction noted in 32%.4
There are several interpretations of oblique dysfunction in exotropia. Jampolsky5, 6 assumed that divergent position of visual axis of the eye allows the development of overaction (or sometimes contracture) of both oblique muscles in divergent eye.
Capo et al7 claimed that the abducting eye would reach the mechanical limit of orbit vertically, although the adducting eye would still be free to move up or down, giving the appearance of both overaction of both obliques. Dysfunction of obliques in fixating eye also can be explained based on the same assumption.
Wilson and Parks4 reported that IOOA had been associated in 32% of 148 patients of intermittent exotropia and IOOA developed at average 5.2 years in these patients. They suggested that IOOA was related with time from onset of strabismus. The mild IOOA had reverted to normal after only horizontal muscle surgery in their patients. In our study, the mean age of subjects was 11.4±7.2 years. We can suspect that long time has lasted since onset of exotropia because intermittent exotropia usually develop during early childhood less than 5–6 years of age. Mild IOOA less than +2 was observed in 61.2% of our subjects.
All these suggestions mean that oblique dysfunction and small hypertropia in exotropia would be secondary phenomenon caused by longstanding divergent situation, as described by others.8, 9, 10 Therefore, small amount of cyclovertical dysfunctions could be disappeared in exotropia when eyes are aligned horizontally by surgical correction of exotropia. It also seems prudent to avoid doing oblique muscle surgery for mild IOOA when seen in conjunction with horizontal strabismus.
Jampolsky11 mentioned that the most common cause of positive Bielschowsky head tilt test is contracture of SR muscle. Mild vertical deviation in combination with long-lasting dysfunction of obliques might induce SR contracture and cause positive Bielschowsky head tilt test in our subjects. We assume that overaction of cyclovertical muscle was mild and transient in long-lasting exotropia in our patients, and could be recovered to normal when eyes are aligned horizontally.
Kushner1 reported seven patients of hypertropia with intermittent exotropia, who had simulated SOP. He gave warning to doing vertical surgery in such patients and recommended prism adaptation test, which may be helpful in predicting the disappearance of hypertropia.
We assume that mild SO underaction was due to relaxation of the antagonist of overacting IO based upon Sherrington’s law and also seems transient phenomenon. It would gradually normalize in some time after surgery. In our study, 27 patients with hypertropia more than 10 PD in primary gaze resembled SOP; however, more than 10 PD hypertropia was even ameliorated by horizontal muscle surgery only.
Many reports described the characteristics of SOP including torticollis, facial asymmetry, marked underaction of SO, large vertical fusional amplitudes, and associated horizontal strabismus. Torticollis is the most frequent cause for presentation to the ophthalmologist.12, 13, 14 In our study, we excluded the patients with characteristics of SOP and any of them did not manifest SOP after horizontal muscle surgery. The vertical deviation could be disappeared spontaneously if exotropia is corrected after horizontal muscle surgery only.
When exotropia persisted for a long time, elevators such as IO or SR would overact easily in exoposition of eye rather than depressors. The action of depressors may be protected by anatomical structures like lockwood ligament in the lower part of eye. However, depressors would gradually overact. Finally, all oblique dysfunctions can be resulted in long-standing exotropia.
In our patients with intermittent exotropia, hypertropia up to 14 PD in primary gaze was ameliorated spontaneously after horizontal muscle surgery only.
In conclusion, in the patients showing exotropia with small amount of concomitant hypertropia or oblique dysfunction, surgeons should be cautious in doing cyclovertical muscle surgery because hypertropia or oblique dysfunction can be vanished after horizontal muscle surgery only. Careful examinations for prominent underaction of SO, foveal extorsion, subjective and objective degree of torsion, and other characteristics of SOP are needed.
References
Kushner BJ . Simulated superior oblique palsy. Ann Ophthalmol 1981; 13 (3): 337–343.
Moore S, Stockbridge L, Knapp P . A panoramic view of exotropia. Am Orthopt J 1977; 27: 70–79.
Davis GT . Vertical deviations associated with exodeviations. In: Manley DR (ed). Symposium on Horizontal Ocular Deviations. CV Mosby: St Louis, 1971, pp 149–156.
Wilson ME, Parks MM . Primary inferior oblique overaction in congenital esotropia, accommodative esotropia, and intermittent exotropia. Ophthalmology 1989; 96: 950–957.
Jampolsky A . Bilateral anomalies of the oblique muscles. Trans Amer Acad Ophthalmol Otolaryng 1957; 61: 689–697.
Jampolsky A . Treatment of exodeviations. In: Conway MD (ed). Transactions of the New Olreans Academy of Ophthalmology: Pediatric Ophthalmology and Strabismus. Raven: New York, NY, 1986, pp 201–234.
Capo H, Mallette RA, Guyton DL . Overacting oblique muscles in exotropia. A mechanical explanation. J Pediatr Ophthalmol Strabismus 1988; 25: 281–285.
Noorden GK . Binocular Vision and Ocular Motility, 6th edn. Mosby-year Book: St Louis, MO, 2002; 396pp.
Crawford JS, Smith DR . Strabismus. In: Crawford JS, Morin JD (eds). The Eye in Childhood. Grune & Stratton: New York, NY, 1983; 64–80.
Mein J, Harcourt B . Diagnosis and Management of Ocular Motility Disorders. Blackwell Scientific: Oxford, 1986, 204pp.
Jampolsky A . Management of vertical strabismus. In: Conway MD (ed). Transactions of the New Olreans Academy of Ophthalmology: Pediatric Ophthalmology and Strabismus. Raven: New York, 1986, pp 141–171.
von Noorden GK, Murray E, Wong SY . Superior oblique paralysis. A review of 270 cases. Arch Opthalmol 1986; 104: 1771–1776.
Helveston EM, Krach D, Plager DA, Ellis FD . A new classification of superior oblique palsy based on congenital variations in the tendon. Ophthalmology 1992; 99: 1609–1615.
Tarczy-Hornoch K, Repka MX . Superior oblique palsy or paresis in pediatrc patients. J AAPOS 2004; 8 (2): 133–140.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cho, Y., Kim, SH. Surgical outcomes of intermittent exotropia associated with concomitant hypertropia including simulated superior oblique palsy after horizontal muscles surgery only. Eye 21, 1489–1492 (2007). https://doi.org/10.1038/sj.eye.6702585
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702585