Abstract
Purpose
To ascertain the conjunctival bacterial pattern of diabetics undergoing cataract operation to reduce the risk of postoperative endophthalmitis (PE).
Methods
An observational retrospective study of the conjunctival bacteria of consecutive patients undergoing cataract surgery from July 2005 to November 2008. Records of patients having eye surgical prophylaxis in the 6 months before the culture and those patients having cataract operation combined with other surgical procedures were excluded. Aerobic and microaerobic cultures were carried out. Dade-Behring panels were used for bacterial identification. The database containing the isolated bacteria was linked to another Access database containing demographic and clinical data such as diabetes presence and baseline blood glucose and creatinine levels. The conjunctival bacteria of diabetics were compared with those of the non-diabetics. Epidat 3.1 program was used for statistical calculations.
Results
From 5922 selected patients, 1325 (22.37%) knew they were diabetics (higher prevalence than expected). Among self-reported non-diabetics, 900 (15.2%) could be ‘unknown’ diabetics; another 274 had an impaired renal function; and 3423 non-diabetics joined the control group. Diabetics have a significantly higher prevalence of Staphylococcus aureus, Enterococci, certain Streptococci, and Klebsiellasp. than non-diabetics. Diabetics and non-diabetics having a blood creatinine level above 105.2 μmol/l had an increased conjunctival bacterial prevalence; these groups had a higher mean age and men predominated.
Conclusions
Diabetics have a conjunctival flora pattern whose increased bacteria are a predominant cause of many diabetic infections. An abnormally high blood creatinine level is an indicator of increased conjunctival colonisation in diabetics and non-diabetics.
Similar content being viewed by others
Introduction
The visual outcome of diabetic patients after postoperative endophthalmitis (PE) is worse than that of non-diabetics.1, 2, 3 In developed countries, there is the threat of an epidemic growth of diabetes prevalence,4, 5, 6 in particular in the elderly; only in the US estimates,4 about 25% of people over 60 years of age will be diabetic (22.6 million people) in the year 2031. In fact, 21.6% of adults older than 65 years had diabetes in the US National Health and Nutrition Examination Survey 1999–2002.7 This age range is also the lifetime period when most patients need to be operated on for cataracts.2, 8, 9 This potential quantity of patients threatened with a poor visual acuity is a reason for preventing diabetics from PE. But, in addition, among the huge quantity of patients undergoing cataract operation, an increased PE incidence has often been associated with diabetes;10, 11, 12, 13, 14 however, not many studies have been carried out to assess this fact and its causes.
Thus, the proportion of diabetics operated on for cataract in the Endophthalmitis study of the European Society of Cataract and Refractive Surgeons15 is unpublished. Although diabetics were included in this study,15 some of the diabetics could be excluded following their exclusion criteria,16 such as the existence of certain ocular and skin infections. This outstanding study15, 17 has stated that certain prophylaxes are capable of reducing the PE incidence after cataract surgery significantly. But, in another study18 with a similar prophylaxis and a less restrictive inclusion criteria of the patients, a wider bacterial spectrum was isolated from their PE cases.19 Other studies of cataract operations carried out in outpatient surgical units20, 21 generated a PE incidence as low as in the mentioned studies17, 18 without using intracameral antibiotics; but possibly the health status of the patients operated on in outpatient units is better than in a tertiary hospital.
Probably, many of the patients operated on for cataracts do no need any prophylaxis, but, at the moment, we cannot identify them. Nevertheless, we can identify patients with an increased risk of PE. Thus, the aim of this study is to ascertain whether the conjunctival flora of diabetic patients undergoing cataract surgery present some peculiarity that could offer some explanation for the often found association of diabetes and PE, apart from the known susceptibility of diabetics with retinopathy for having posterior capsular rupture during the cataract operation,22 as not many of these surgical complications become a PE case.15 For this purpose, we compare the conjunctival bacteria of diabetics and non-diabetics who underwent cataract operation in our tertiary referral hospital.
Materials and methods
Study design
A retrospective observational study of consecutive cases of patients registered in the Laboratory database from 11 July 2005 to 3 November 2008 to have a routine conjunctival culture carried out before their cataract surgery. This database contains the clinical record numbers and demographic data of the patients, the identification, origin and collecting date of the samples, and the results of the microbiological isolations. Every patient undergoing their first cataract operation in our hospital has a preoperative examination carried out, consisting of a thorax X-ray, a basic clinical analysis, a conjunctival bacterial culture, and a clinical evaluation for anaesthetic and surgical purposes (the appointments of this culture and clinical evaluation being on the same day and as close as possible to the scheduled cataract operation date). In this evaluation, performed by the Internist of our Ophthalmic Institute, an Access database is generated, which contains the clinical record number, the surgical procedure indication, the evaluation date, the demographic data and existence of diabetes or not, the kind of diabetes, and the updated baseline blood glucose and creatinine levels, among many other data. As a rule, patients admitted for cataract operations in our hospital and having coexisting dacryocystitis, pterygium, or eyelid closure disturbances are scheduled for the corrections of these coexisting local problems in a separate procedure before the cataract surgery.
The Internal Medicine database was linked to the above mentioned Laboratory database after applying the following exclusion criteria: (i) The Laboratory records of any subsequent cataract operations after the first study record were excluded to avoid the effect of any previous prophylaxis on the conjunctival flora. (ii) Patients having combined surgical procedures of cataract phacoemulsification with trabeculectomy or pars plana vitrectomy were excluded, because of the difficulty of collecting these patients’ samples in the same conditions as in the planned cataract surgeries.
Diabetic and non-diabetic definition criteria: the diabetic condition was self-reported by the patient and the non-diabetic theoretical status. The kind of diabetes was typified by the Internist, based on the updated data and the patient history disease, when it was possible. For classifying the non-diabetic patients, the updated blood glucose level was taken into account because of the impossibility of checking whether an unexpected baseline blood glucose level higher than the upper limit of our normal reference value, 6.05 mmol/l (110 mg per 100 ml), for a non-diabetic patient was true or false. In addition, self-reported non-diabetics having a blood creatinine level >105.2 μmol/l (1.19 mg per100 ml) were studied as a separate group, in order to ensure that false non-diabetics with renal dysfunction did not join the non-diabetic group (in our country, about 23% of the patients suffering from advanced chronic kidney insufficiency are diabetics23, 24). For these reasons, only self-reported non-diabetics having the baseline glucose and creatinine blood levels below the upper limit of our normal reference values were considered for the non-diabetic control group.
Microbiological methods
The specimen collection and the culture technique were described elsewhere.19, 25.The identification of the isolated bacteria was performed as follows: for rapid growing and non-exigent bacteria, Dade-Behring identification panels were used (for Staphylococci and Enterococci, panel PC23; for Gram-negative rods, panels PC38 and PUC37). These panels were automatically read and recorded in the AutoScan4 microbiological system (Siemens Healthcare Systems, Barcelona, Spain). When <5 colony-forming units of a particular coagulase-negative Staphylococcus were isolated, the panel PC23 was used for identification, only if the fermentation mannitol test was positive. The identification of Haemophilus, Neisseria, and Moraxella was carried out with the HNID Dade-Behring panel. Streptococci, Propionibacteria, Corynebacteria, and other Gram-positive rods were identified by their growing characteristics and their macroscopic and microscopic morphology; Streptococcus pneumoniae was differentiated by the optochin disc.
Analysis of the results
In the AutoScan4 microbiological system, a Laboratory data text file was generated, which was exported to a Microsoft Access database (version 2003). This Laboratory database was linked to the Access Internal Medicine database through the clinical record number of the patients. By means of the Access utilities, patients’ records were selected according to the inclusion criteria study. The frequencies of diabetic and non-diabetic patient groups, the mean age of these patient groups, and the isolated conjunctival bacteria of each group were also obtained with the Access program utilities. The isolated bacteria were grouped in order to try to reach a number of bacteria sufficient for making statistical comparisons. The Epidat program 3.1 version (produced by the Pan American Health Organization, Washington, DC, USA and the Consejería de Sanidad de la Junta de Galicia, La Coruña, Spain; http://dxsp.sergas.es), was used for (i) calculating the 95% confidence interval (CI) of the bacterial group percentages in the whole sample of patients. (ii) Comparing the mean age and the percentage of men and women of the non-diabetics control group with that of each of the following groups: self-reported non-diabetics who had a blood creatinine level >105.2 μmol/l; self-reported non-diabetics who had a baseline glycaemia >6.05 mmol/l; diabetics maintaining a creatinine level below 106 μmol/l; those diabetics having a probable renal dysfunction; those identified as type I diabetics; those identified as type II diabetics; those diabetics that we were unable to classify; and those of the whole self-reported diabetics group; also, comparing the mean age of the men and the women of every group of patients in Table 1. (iii) Comparing the conjunctival bacterial percentages of the whole self-reported non-diabetics group with those of the whole self-reported diabetic group. In addition, the conjunctival bacterial percentages of the non-diabetic control group were compared with those of the different groups of diabetics and non-diabetics listed above.
Results
A total of 5922 patients were selected from the linked database according to the inclusion criteria of the study; the mean age of these patients was 73. 66 years, with a standard deviation (SD) of 9.40, in a range from 10 to 98. In all, 3214 (54.27%) of them were women, and 1325 of the patients said that they were diabetic (22.37%); among those diabetics, 191 were identified as type I, 1067 as type II, and 67 were unclassified. The self-reported non-diabetics accounted for 4597 patients; of those, 3423 presented a baseline blood glucose level lower than 6.11 mmol/l and a blood creatinine level below 106 μmol/l (these being the control group); 900 of those self-reported non-diabetics (15.2% of the total sample of patients) who had a fasting glycaemia above 6.05 mmol/l could be diabetics without knowing it; and 362 self-reported non-diabetics had a blood creatinine level >105.2 μmol/l.
In Table 1, the frequency of both sexes, the mean age, the SD, and the range of age of each of the study groups of patients are shown. The significant higher proportion of men in the diabetic and non-diabetic groups with an impaired renal function should be noted, as well as the significant increased age of these two groups of patients, whether men or women, with respect to the control group. Women were older than men in every group, but statistical significance was only found in those groups containing >361 patients. The diabetics type I was the sole group of patients with a mean age lower than the control group.
In Table 2, the whole patients’ conjunctival bacterial frequency and their CI percentages of every bacterial group are given, as well as the frequency of these bacteria in the whole self-reported diabetic and non-diabetic groups. There are eight groups of conjunctival bacterial colonisers of the diabetic patient group outside the CI of the bacterial percentages of the whole 5922 patients studied. From these eight bacterial groups, four turnd out to be statistically higher than those for the whole self-reported non-diabetic, which are Staphylococcus aureus, Enterococci, Streptococci (except S. pneumoniae), and Klebsiella sp.
Table 3 shows the comparison of the control group's conjunctival bacterial percentages with those of the following groups: the self-reported non-diabetics having a fasting glycaemia >6.05 mmol/l; the self-reported non-diabetics having a blood creatinine level >105.2 μmol/l; the diabetic patients who had a blood creatinine level <106 μmol/l; and the diabetics having a creatinine level >105.2 μmol/l. In this table, both groups of diabetics and non-diabetics having an impaired renal function exhibited a significantly higher percentage of S. aureus and other Staphylococci. In the two groups of diabetics, the S. aureus and Klebsiella sp. prevalence are significantly higher than those in the non-diabetics control group.
In Table 4, the conjunctival bacterial percentages of the non-diabetic control group were compared with those of the following groups: diabetics type I, diabetics type II, unclassified diabetics, and all the self-reported diabetics. Diabetics types I and II coincided in having a higher prevalence of S. aureus and Klebsiella sp., and a significantly lower prevalence of sterile cultures, compared with those in the control group, although the S. aureus prevalence of diabetics type I did not reach statistical significance.
In Table 5, the proportion of non-diabetics and different kinds of diabetics who had an impaired renal function when they underwent cataract surgery is shown.
Discussion
To our knowledge, this study provides the biggest sample of patients ever described for studying the conjunctival bacterial pattern in diabetics. The prevalence of the 900 self-reported non-diabetics (15.2% of the total sample of patients) excluded from the control group because of the uncertainty that they could be ‘unknown’ diabetics, is a result consistent with the prevalence of ‘unknown’ diabetics in our country.24, 26 The 22.37% of our patients who knew that they were diabetics when they underwent cataract operation in our hospital is a higher prevalence of ‘known’ diabetes than the national prevalence average of our country, as it was at the beginning of the last decade.24, 26 In two studies carried out at about the same time, the prevalence of diabetics undergoing cataract surgery was about 11% in the United Kingdom2 and 20% in New Zealand;27 but this difference is probable due to ethnic characteristics.26 Our patients’ increased prevalence could be due to the following reasons. First, the proportion of elderly patients in this study is bigger than that in the above mentioned Spanish studies, and an increase in age was associated with the risk of being diabetic everywhere.4, 5, 6, 7, 24, 26 Second, there could be a concentration of diabetic patients with a poor health status in a tertiary referral hospital as ours. Third, the predicted worldwide tendency of an increasingly serious diabetes epidemic could have already been affecting our country's diabetes prevalence.
The conjunctival bacterial pattern of our diabetics presents the peculiarity of having an increased prevalence of S. aureus, Klebsiella sp., Enterococci, and Streptococci α-haemolytic different from S. pneumoniae with respect to the non-diabetics conjunctival bacteria (Tables 2 and 4). This peculiarity was even detected by comparing the self-reported information of the patients as diabetics or non-diabetics (Table 2). However, the two most consistent of these results is the higher prevalence of S. aureus and Klebsiella sp., found even in those diabetics with a normal blood creatinine level or when the number of patients was smaller, as in diabetics type I or those diabetics with an abnormally high blood creatinine level (Tables 2,3,4). The Enterococci prevalence is higher in all the diabetic groups with respect to the control group; but only when the total group of diabetics is compared, a statistical significance is obtained (Tables 2 and 4). The higher prevalence of Streptococci (except S. pneumoniae) of the diabetics reached statistical significance in some of the groups, but its distribution among groups is not so persistent (Tables 2,3,4).
In one of the two small-sized studies published on the diabetics conjunctival bacteria,28, 29 an increased prevalence of S. aureus was only found in diabetics type II, although the number of patients studied by Bilen et al28 was small (17 diabetics type I, 66 diabetics type II, and 50 control subjects). But only an increased prevalence of SCN was found in the other one,29 which only studies the flora of diabetics with retinopathy. This second study29 used certain exclusion criteria for their patients, such as any sign of external ocular infection or inflammation, which we did not use. In addition, their patients were younger (mean age 67 years) than ours (mean age 73 years), which could condition their flora prevalence.9
Undoubtedly, the great number of patients contained in our sample allows us to identify this diabetic bacterial pattern, although the prevalence of the affected bacteria is not strikingly high. However, our big sample of patients also allows us to differentiate the influence of diabetes on the conjunctival bacterial flora from other factors affecting the prevalence of these flora. In a previous study from our hospital,9 advanced age and male sex increased the conjunctival bacterial prevalence; in this study, this effect is also shown (Tables 1 and 3). But, in addition, the groups of patients having a predominance of men and a higher mean age, both diabetics and non-diabetics, also had a blood creatinine level above the normal level, which indicates that the conjunctival bacterial prevalence is also altered in the patients with a suspected impaired renal function (Tables 1 and 3). In particular, the higher conjunctival prevalence of S. aureus in those patients with a high creatinine level is congruent with the well-known likelihood of diabetics and non-diabetics suffering from nephropathy of being nasal carriers of this bacterium30, 31 and having other infections as a consequence of this carriage.32 This fact reinforced the reliability of the association of an increased conjunctival S. aureus colonisation with a suspected renal lesion in our patients who are diabetic or not.
The prevalence of diabetic nephropathy varies among studies,23, 24, 26, 33, 34, 35but there is some agreement as regard to recognising its determinant factors, such as increased blood pressure,33, 34, 35, 36 increased glycosylated haemoglobin,33, 35, 36 increased blood creatinine,33, 34 male sex,33, 34 and a previous retinopathy.33, 34 The prevalence of retinopathy also varies among studies,24, 26, 34, 35, 37and its development is mainly associated with the duration of the diabetes,35, 37 among other determinant factors. We did not find a fixed rule in the diabetes follow-up studies for the appearance and coincidence of these two diabetic complications.34, 35, 37 However, the concomitance of nephropathy and retinopathy represents a worse state in the diabetes progression.34, 35 This fact indicates that, apart from the risk of diabetics with retinopathy having a higher rate of posterior capsule rupture during the cataract operations22 (a surgical complication associated with an increased incidence of PE15, 18), diabetics with renal function impairment have a potential increased risk of bacterial contamination during that operation. In our study, 14.11% of the self-reported diabetics had an abnormally high blood creatinine level; among those, the proportion in the diabetics type I group is higher than that in the type II group (Table 5). But 7.87% of the self-reported non-diabetics also presented a suspected renal dysfunction, although we do not know what part of them were unknown diabetics. On the basis of our results, 9.27% of the patients with a suspected renal dysfunction had an increased conjunctival bacterial prevalence (Table 5).
On the other hand, a gradual S. aureus conjunctival colonisation (8.78, 11.16, and 15.51%) could be seen in the three groups of differentiated diabetics that could represent three different stages of the diabetes (Table 3). (i) Patients who recently became diabetics (part of those self-reported non-diabetics with a high fasting glycaemia); (ii) diabetics with a normal blood creatinine level; (iii) diabetics with a suspected renal function impairment. The progressive colonisation by Klebsiella sp. and Enterococci in the three groups of diabetics follows the same behaviour as the S. aureus colonisation (Table 3), despite their lower prevalence on the conjunctiva. This progressive colonisation suggests us the possibility that there exists a group of diabetics with a higher conjunctival bacterial load because of the personal development of their disease, which could explain the different risk of PE attributed to diabetes in patients operated on for cataracts. Another point to underline among our data for assessing the diabetic conjunctival bacterial pattern is the fact that patients in the control group had similar sex distribution and mean age to those diabetics with a normal blood creatinine level (Table 1). Therefore, the bacterial pattern of those diabetics cannot be attributed to these two conditions.
However, what is more surprising from our study is to note that diabetes has been described as being a risk for different infections caused by the same bacteria that we have found more prevalent on diabetics’ conjunctiva. For instance, bacteraemia caused by S. aureus,38, 39 Enterococci,40 and Klebsiella sp.;41, 42 hepatic abscess and fascial space infection of the head and neck and soft tissue due to Klebsiella pneumoniae.43, 44 In particular, the association of K. pneumoniae and bloodstream infections of diabetics was described in a recent study,42 in which diabetics had a 4.4-fold higher risk of bloodstream infections than non-diabetics. The repetition of this diabetic bacterial pattern led us to suppose that diabetes provides certain conditions that encourage this bacterial colonisation.
In conclusion, ophthalmic surgeons should be aware that some diabetics have a higher risk of contamination with S. aureus, Enterococci, Klebsiella sp., and certain Streptococci during the cataract surgery compared with the non-diabetics. Among these bacteria, Enterococci present a high antibiotic resistance pattern,19, 45 and this resistance is on the increase in S. aureus.32, 46 An advanced age and an abnormally high blood creatinine level are also associated with an increased conjunctival bacterial colonisation in diabetics and non-diabetics; these two simple figures could be reliable indicators of the contamination risk.

References
Phillips II WB, Tasman WS . Postoperative endophthalmitis in association with diabetes mellitus. Ophthalmology 1994; 101: 508–518.
Desai P, Minassian DC, Reidy A . National cataract survey 1997–8: a report of results of the clinical outcomes. Br J Ophthalmol 1999; 83: 1336–1340.
Doft BH, Wisniewski SR, Kelsey SF, Fitzgerald SG, Endophthalmitis Vitrectomy Study Group. Diabetes and postoperative endophthalmitis in the endophthalmitis vitrectomy study. Arch Ophthalmol 2001; 119: 650–656.
Mainous III AG, Baker R, Koopman RJ, Saxena S, Diaz VA, Everett CJ et al. Impact of the population at risk of diabetes on projections of diabetes burden in the United States: an epidemic on the way. Diabetologia 2007; 50: 934–940.
Frese T, Sandholzer H, Voigt S, Voigt R . Epidemiology of diabetes mellitus in German general practitioners′ consultation—results of the SESAM 2-study. Exp Clin Endocrinol Diabetes 2008; 116: 326–328.
Magliano DJ, Shaw JE, Shortreed SM, Nusselder WJ, Liew D, Barr EL et al. Lifetime risk and projected population prevalence of diabetes. Diabetologia 2008; 51: 2179–2186.
Cowie CC, Rust KF, Byrd-Holt DD, Eberhardt MS, Flegal KM, Engelgau MM et al. Prevalence of diabetes and impaired fasting glucose in adults in the US population: National Health And Nutrition Examination Survey 1999–2002. Diabetes Care 2006; 29: 1263–1268.
West ES, Behrens A, McDonnell PJ, Tielsch JM, Schein OD . The incidence of endophthalmitis after cataract surgery among the US Medicare population increased between 1994 and 2001. Ophthalmology 2005; 112: 1388–1394.
Rubio EF . Influence of age on conjunctival bacteria of patients undergoing cataract surgery. Eye 2006; 20: 447–454.
Kattan HM, Flynn HW, Pflugfelder SC, Robertson C, Foster RK . Nosocomial endophthalmitis survey. Current incidence of infection after intraocular surgery. Ophthalmology 1991; 98: 227–238.
Chitkara DK, Smerdon DL . Risk factors, complications, and results in extracapsular cataract extraction. J Cataract Refract Surg 1997; 23: 570–574.
Ozer-Arasli A, Schwenn O, Dick B, Pfeiffer N . Endophthalmitis after cataract surgery: long-term follow-up. Klin Monatsbl Augenheilkd 1997; 211: 178–182.
Schmitz S, Dick HB, Krummenauer F, Pfeiffer N . Endophthalmitis in cataract surgery: results of a German survey. Ophthalmology 1999; 106: 1869–1877.
Zell K, Engelmann K, Bialasiewicz AA, Richard G . Endophthalmitis after cataract surgery: predisposing factors, infectious agents and therapy. Ophthalmologe 2000; 97: 257–263.
Barry P, Seal DV, Gettinby G, Lees F, Peterson M, Revie CW, ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: preliminary report of principal results from a European multicenter study. J Cataract Refract Surg 2006; 32: 407–410.
Seal DV, Barry P, Gettinby G, Lees F, Peterson M, Revie CW, et al., ESCRS Endophthalmitis Study Group. ESCRS study of prophylaxis of postoperative endophthalmitis after cataract surgery: case for a European multicenter study. J Cataract Refract Surg 2006; 32: 396–406.
Endophthalmitis Study Group, European Society of Cataract and Refractive Surgeons. Prophylaxis of postoperative endophthalmitis following cataract surgery: results of the ESCRS multicenter study and identification of risk factors. J Cataract Refract Surg 2007; 33: 978–988.
Lundstrom M, Wejde G, Stenevi U, Thorburn W, Montan P . Endophthalmitis after cataract surgery: a nationwide prospective study evaluating incidence in relation to incision type and location. Ophthalmology 2007; 114: 866–870.
Fernández-Rubio E, Urcelay JL, Cuesta-Rodriguez T . The antibiotic resistance pattern of conjunctival bacteria: a key for designing a cataract surgery prophylaxis. Eye 2009; 23: 1321–1328.
Bohigian GM . A retrospective study of the incidence of culture-positive endophthalmitis after cataract surgery and the use of preoperative antibiotics. Ophthalmic Surg Lasers Imaging 2007; 38: 103–106.
Lloyd JC, Braga-Mele R . Incidence of postoperative endophthalmitis in a high-volume cataract surgicentre in Canada. Can J Ophthalmol 2009; 44: 288–292.
Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye 2009; 23: 31–37.
Ceballos M, López-Revuelta K, Saracho R, García López F, Castro P, Gutiérrez JA et al. Dialysis and transplant patients Registry of the Spanish Society of Nephrology. Nefrologia 2005; 25: 121–124, 126–129.
Goday A . Epidemiology of diabetes and its non-coronary complications. Rev Esp Cardiol 2002; 55: 657–670.
Rubio EF . Climatic influence on conjunctival bacteria of patients undergoing cataract surgery. Eye 2004; 18: 778–784.
Goday A, Serrano-Ríos M . Epidemiology of diabetes mellitus in Spain. Critical review and new perspectives. Med Clin (Barc) 1994; 102: 306–315.
Riley AF, Malik TY, Grupcheva CN, Fisk MJ, Craig JP, McGhee CN . The Auckland cataract study: comorbidity, surgical techniques, and clinical outcomes in a public hospital service. Br J Ophthalmol 2002; 86: 185–190.
Bilen H, Ates O, Astam N, Uslu H, Akcay G, Baykal O . Conjunctival flora in patients with type 1 or type 2 diabetes mellitus. Adv Ther 2007; 24: 1028–1035.
Martins EN, Alvarenga LS, Höfling-Lima AL, Freitas D, Zorat-Yu MC, Farah ME et al. Aerobic bacterial conjunctival flora in diabetic patients. Cornea 2004; 23: 136–142.
Luzar MA, Coles GA, Faller B, Slingeneyer A, Dah GD, Briat C et al. Staphylococcus aureus nasal carriage and infection in patients on continuous ambulatory peritoneal dialysis. N Engl J Med 1990; 322: 505–509.
Lederer SR, Riedelsdorf G, Schiffl H . Nasal carriage of meticillin resistant Staphylococcus aureus: the prevalence, patients at risk and the effect of elimination on outcomes among outclinic haemodialysis patients. Eur J Med Res 2007; 12: 284–288.
Safdar N, Bradley EA . The risk of infection after nasal colonization with Staphylococcus aureus. Am J Med 2008; 121: 310–315.
Retnakaran R, Cull CA, Thorne KI, Adler AI, Holman RR, UKPDS Study Group. Risk factors for renal dysfunction in type 2 diabetes: UK Prospective Diabetes Study 74. Diabetes 2006; 55: 1832–1839.
Alwakeel JS, Al-Suwaida A, Isnani AC, Al-Harbi A, Alam A . Concomitant macro and microvascular complications in diabetic nephropathy. Saudi J Kidney Dis Transpl 2009; 20: 402–409.
Romero P, Salvat M, Fernández J, Baget M, Martinez I . Renal and retinal microangiopathy after 15 years of follow-up study in a sample of type 1 diabetes mellitus patients. J Diabetes Complications 2007; 21: 93–100.
Poulter NR . Blood pressure and glucose control in subjects with diabetes: new analyses from ADVANCE. J Hypertens 2009; 27 (Suppl 1): S3–S8.
Salti HI, Nasrallah MP, Taleb NM, Merheb M, Haddad S, El-Annan J et al. Prevalence and determinants of retinopathy in a cohort of Lebanese type II diabetic patients. Can J Ophthalmol 2009; 44: 308–313.
Laupland KB, Ross T, Gregson DB . Staphylococcus aureus bloodstream infections: risk factors, outcomes, and the influence of methicillin resistance in Calgary, Canada, 2000–2006. J Infect Dis 2008; 198: 336–343.
Khatib R, Johnson LB, Sharma M, Fakih MG, Ganga R, Riederer K . Persistent Staphylococcus aureus bacteremia: incidence and outcome trends over time. Scand J Infect Dis 2009; 41: 4–9.
Poh CH, Oh HM, Tan AL . Epidemiology and clinical outcome of enterococcal bacteraemia in an acute care hospital. J Infect 2006; 52: 383–386.
Akbar DH . Adult bacteremia. Comparative study between diabetic and non-diabetic patients. Saudi Med J 2000; 21: 40–44.
Stoeckle M, Kaech C, Trampuz A, Zimmerli W . The role of diabetes mellitus in patients with bloodstream infections. Swiss Med Wkly 2008; 138: 512–519.
Han SH . Review of hepatic abscess from Klebsiella pneumoniae. An association with diabetes mellitus and septic endophthalmitis. West J Med 1995; 162: 220–224.
Chang CM, Lu FH, Guo HR, Ko WC . Klebsiella pneumoniae fascial space infections of the head and neck in Taiwan: emphasis on diabetic patients and repetitive infections. J Infect 2005; 50: 34–40.
Sood S, Malhotra M, Das BK, Kapil A . Enterococcal infections & antimicrobial resistance. Indian J Med Res 2008; 128: 111–121.
Freidlin J, Acharya N, Litman TM, Cevallos V, Whitcher JP, Margolis TP . Spectrum of eye disease caused by methicillin-resistant Staphylococcus aureus. Am J Ophthalmol 2007; 144: 313–315.
Acknowledgements
The authors thank María Luisa Martinez, MD, for providing a part of the instrumentation needed; José Antonio Tintó, MD, who collected part of the data; José Ma Bellón, Hospital Statistician, for statistical revision; Ana Almazán, María-José Castaño, and María-Carmen Navarro, for technical help; Roberto Pozo for help with some of the Access program utilities; and David Frost for his assistance with the English translation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fernández-Rubio, M., Rebolledo-Lara, L., Martinez-García, M. et al. The conjunctival bacterial pattern of diabetics undergoing cataract surgery. Eye 24, 825–834 (2010). https://doi.org/10.1038/eye.2009.218
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/eye.2009.218
Keywords
This article is cited by
-
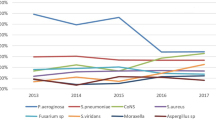
Changes in the preoperative ocular surface flora with an increase in patient age: A surveillance analysis of bacterial diversity and resistance to fluoroquinolone
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Conjunctival sac bacterial culture of patients using levofloxacin eye drops before cataract surgery: a real-world, retrospective study
BMC Ophthalmology (2022)
-
Bacterial distribution on the ocular surface of patients with primary Sjögren’s syndrome
Scientific Reports (2022)
-
Cataract Surgery Considerations for Diabetic Patients
Current Diabetes Reports (2021)
-
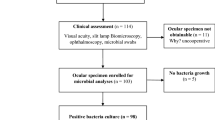
Positive bacterial culture in conjunctival sac before cataract surgery with night stay is related to diabetes mellitus
BMC Ophthalmology (2017)